Complex Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a minimally invasive procedure used to treat blocked or narrowed coronary arteries, which can lead to conditions such as angina or myocardial infarction (heart attack). In cases where the blockages are severe or located in challenging anatomical regions, advanced techniques in complex angioplasty have emerged to improve procedural success rates and patient outcomes.
These advanced techniques encompass a range of innovative strategies and technologies that allow for the successful treatment of complex coronary artery disease.
Comprehensive Techniques in Complex Coronary Angioplasty
Complex angioplasty refers to the minimally invasive procedure used to treat complex coronary artery disease (CAD), which involves the presence of multiple blockages, long and diffuse lesions, bifurcation lesions, chronic total occlusions (CTOs), or calcified lesions. These cases often require advanced techniques to encompass a range of innovative strategies and technologies for a successful treatment.
Chronic Total Occlusion (CTO) Intervention
CTO intervention involves the treatment of completely blocked coronary arteries that have been occluded for an extended period. Advanced techniques, such as retrograde approaches, subintimal tracking and re-entry, and dedicated CTO guidewires and microcatheters, enable interventional cardiologists to navigate and successfully recanalize these challenging lesions.
This advanced technique in complex angioplasty has been associated with improved patient symptoms, left ventricular function, and long-term survival.
Bifurcation Lesion Treatment
Bifurcation lesions occur when a coronary artery divides into two branches, and the plaque buildup is present at the bifurcation site. Advanced techniques, such as provisional stenting, two-stent techniques (culotte, T-stenting, and kissing), and dedicated bifurcation stents, allow for precise and optimized treatment of these complex lesions.
The goal is to maintain good blood flow to both branches while ensuring optimal stent placement and expansion.
Rotational Atherectomy
Rotational atherectomy is a technique used for complex coronary angioplasty to treat heavily calcified coronary lesions. It involves the use of a high-speed rotating burr that grinds away the calcified plaque, allowing for better stent deployment and expansion.
Advanced rotational atherectomy devices with improved cutting efficiency and safety profiles have been developed, enabling successful treatment of even the most calcified lesions.
Intravascular Imaging
Intravascular imaging techniques, such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), provide detailed and precise imaging of the coronary arteries during angioplasty procedures.
These imaging modalities of complex coronary angioplasty allows for better lesion characterization, accurate stent sizing, and optimization of stent deployment. They help interventional cardiologists assess the quality of stent expansion and identify potential complications, leading to improved procedural outcomes.
Benefits of Advanced Techniques
Advanced techniques in complex coronary angioplasty offer several benefits, enhancing the effectiveness and safety of the procedure. Some of them include:
Increased Procedural Success
Advanced techniques in complex coronary angioplasty have significantly improved procedural success rates. The ability to navigate and treat challenging lesions, such as chronic total occlusions or bifurcation lesions, increases the likelihood of achieving complete revascularization and restoring blood flow to the heart. This translates into improved symptom relief, reduced angina, and enhanced quality of life for patients.
Reduced Need for Surgery
By successfully treating complex lesions that were traditionally considered surgical cases, advanced techniques in complex angioplasty have reduced the need for bypass surgery in many patients. This means fewer complications associated with surgery, shorter hospital stays, and quicker recovery times for patients.
Improved Long-Term Outcomes
Advanced techniques of complex coronary angioplasty such as CTO intervention and intravascular imaging, have been associated with improved long-term outcomes. Successful recanalization of chronic total occlusions can improve left ventricular function and reduce the risk of heart failure. Intravascular imaging allows for precise stent placement, reducing the risk of stent thrombosis and restenosis, which can lead to repeat procedures.
Minimally Invasive Approach
One of the key advantages of advanced techniques in complex angioplasty is their minimally invasive nature. Compared to traditional open-heart surgery, angioplasty procedures involve small incisions or punctures, leading to less pain, reduced scarring, and faster recovery times for patients.
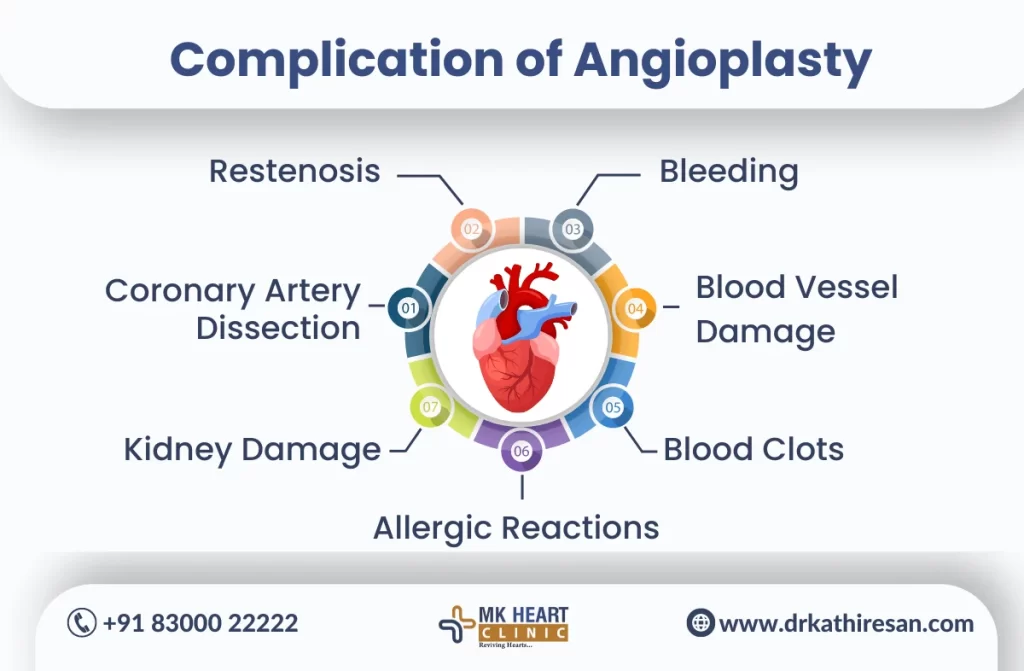
Risks of Complex Coronary Angioplasty
Complex Coronary Angioplasty, a critical intervention for treating coronary artery disease, entails certain risks that individuals should be aware of:
- Bleeding and Hematoma: Complex Coronary Angioplasty may pose a risk of bleeding at the catheter insertion site, leading to hematoma formation.
- Vascular Complications: The procedure can result in damage to blood vessels, potentially causing narrowing or blockages, emphasizing the importance of an experienced medical team in Complex Coronary Angioplasty.
- Allergic Reactions: Contrast dye used during the procedure may trigger allergic reactions in some individuals, necessitating careful pre-assessment.
- Restenosis: Despite successful angioplasty, there is a risk of restenosis, where the treated artery may narrow again over time, requiring additional interventions.
- Coronary Artery Dissection: Complex procedures increase the likelihood of coronary artery dissection, a tear in the artery wall, necessitating prompt medical attention.
- Thrombosis: Blood clot formation at the stent site, known as stent thrombosis, is a potential risk, highlighting the need for antiplatelet medications post-procedure.
- Kidney Damage: Contrast dye usage may impact kidney function, especially in individuals with pre-existing kidney issues.
- Infection: Though rare, infections at the catheter insertion site may occur, underscoring the importance of maintaining sterile conditions during Complex Coronary Angioplasty.
Understanding these risks associated with Complex Coronary Angioplasty allows individuals to make informed decisions about their cardiac care, emphasizing the need for thorough pre-procedural assessments and a skilled medical team to navigate these challenges effectively.
Conclusion
To conclude, advanced techniques in complex coronary angioplasty have revolutionized the treatment of challenging coronary artery disease. These techniques offer interventional cardiologists the tools and strategies necessary to successfully navigate and treat complex lesions, leading to improved procedural success rates, reduced need for surgery, and better long-term outcomes for patients.
Moreover, the continued advancement of these techniques holds great promise in further enhancing the effectiveness and safety of coronary angioplasty procedures.


