Heart failure is a complex condition that can disrupt daily life, but with the right heart failure treatments, individuals can manage symptoms and enhance well-being. At Dr. Kathiresan’s clinic, we take a personalized approach to heart failure treatments, including the treatment of anemic heart failure, helping patients strengthen their heart, alleviate symptoms, and support long-term health. By understanding the underlying causes, recognizing symptoms, and exploring various treatment options, patients can actively manage chronic heart failure symptoms for a better quality of life.
Understanding Heart Failure
Heart failure happens when the heart’s ability to pump blood weakens, affecting the supply of oxygen and nutrients throughout the body. It can develop gradually or suddenly, and early intervention is essential to prevent further complications.
- Decreased oxygen supply to vital organs
- Possible fluid accumulation in the lungs, abdomen, or limbs
- Often related to conditions such as coronary artery disease or hypertension
Proper heart failure treatments can reduce symptoms and help maintain heart health.
Types of Heart Failure
Understanding the types of heart failure is crucial for tailoring treatment plans:
- Left-sided heart failure: The most common type, where the heart can’t pump enough oxygen-rich blood to the body.
- Right-sided heart failure: Often caused by left-sided failure, leading to fluid buildup in the abdomen and legs.
- Diastolic heart failure: The heart muscles become stiff, reducing their ability to fill and pump effectively.
- Systolic heart failure: The heart muscle weakens and can’t pump blood efficiently.
Customized heart failure treatments at Dr. Kathiresan’s clinic address each type to ensure optimal outcomes.
Symptoms of Heart Failure
Identifying chronic heart failure symptoms early can enable timely treatment. These symptoms often affect everyday activities and can range in severity. Common signs include:
- Shortness of breath during physical activity or while lying flat
- Chronic coughing or wheezing, sometimes producing mucus
- Swelling in the feet, ankles, or abdomen
- Persistent fatigue or weakness, even with sufficient rest
- Rapid or irregular heartbeat
Being aware of these chronic heart failure symptoms allows individuals to seek effective heart failure treatments that relieve discomfort and support overall heart health. treatments that relieve discomfort and support overall heart health.
Primary Causes of Heart Failure
Knowing the root causes of heart failure is essential for prevention and treatment. At Dr. Kathiresan’s clinic, we prioritize early identification of risk factors to improve patient outcomes. Major contributing factors include:
- Coronary artery disease (CAD): Narrowed arteries restrict blood flow to the heart, weakening it over time.
- High blood pressure: Sustained high pressure makes the heart work harder, eventually reducing its efficiency.
- Heart attack: Sudden blood loss damages the heart muscle, sometimes irreversibly.
- Diabetes: Raises the risk of heart conditions, often leading to heart failure.
Addressing these risk factors early through customized heart failure treatments can slow the progression and improve heart function.
Risk Factors for Heart Failure
Understanding the risk factors helps in preventing or managing heart failure effectively:
- Chronic Conditions: Hypertension, diabetes, and coronary artery disease increase the likelihood of heart failure.
- Lifestyle Choices: Poor diet, lack of exercise, and smoking are significant contributors.
- Age and Gender: Older adults and men are more prone to heart failure, though women experience unique symptoms.
- Anemia: This condition can exacerbate heart failure, necessitating the treatment of anemic heart failure to manage symptoms effectively.
Identifying and addressing these risks early can significantly reduce the progression of heart failure.
Diagnosis of Heart Failure
Diagnosing heart failure involves a combination of physical exams, medical history evaluations, and diagnostic tests. Common procedures include:
- Physical Examination: Doctors check for symptoms like swelling in the legs, irregular heartbeats, or difficulty breathing.
- Blood Tests: Help detect conditions like anemia or thyroid issues contributing to heart failure.
- Echocardiogram: A detailed ultrasound of the heart to assess its structure and function.
- Chest X-ray: Identifies fluid buildup or enlargement of the heart.
- Electrocardiogram (ECG): Tracks the heart’s electrical activity, detecting irregular rhythms.
For patients experiencing chronic heart failure symptoms like fatigue, shortness of breath, or swelling, early diagnosis is critical for initiating effective heart failure treatments.
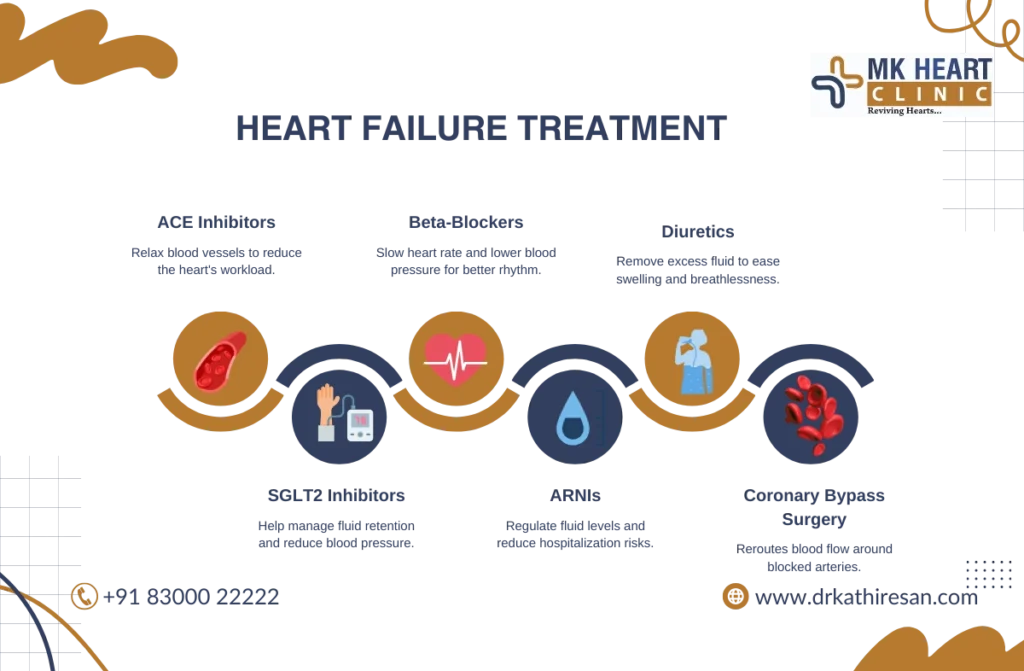
Treatment Options for Heart Failure
Treating heart failure requires a variety of strategies, from medications to surgical interventions, each focused on improving heart function and relieving symptoms.
Medications for Heart Failure
- ACE Inhibitors and ARBs: Relax blood vessels, reducing the heart’s workload and lowering blood pressure.
- Beta-blockers: Slow the heart rate, reduce blood pressure, and minimize abnormal rhythms.
- Diuretics: Remove excess fluid buildup, easing symptoms like swelling and breathlessness.
- SGLT2 Inhibitors: Initially used for diabetes, now recognized for reducing blood pressure and fluid retention in heart failure patients.
- Digoxin: Increases the strength of each heartbeat to relieve severe symptoms such as fatigue.
- ARNIs (Angiotensin Receptor-Neprilysin Inhibitors): Regulate fluid and reduce hospitalizations in heart failure patients.
Living with Heart Failure
Managing heart failure requires lifestyle adjustments and medical care to improve quality of life. Here’s how:
- Follow Prescribed Medications – Essential for managing symptoms and preventing complications.
- Monitor Symptoms Regularly – Watch for swelling, fatigue, or shortness of breath.
- Maintain a Low-Sodium Diet – Helps control fluid retention and reduce strain on the heart.
- Stay Physically Active – Light exercise improves circulation and heart function.
- Manage Stress – Relaxation techniques like meditation support heart health.
- Monitor Fluid Intake – Excess fluids can worsen heart failure symptoms.
- Regular Doctor Visits – Essential for tracking progress and adjusting heart failure treatments as needed.
While heart failure is a chronic condition, proper management, including lifestyle changes and advanced heart failure treatments, can help patients lead a fulfilling life. Consulting a cardiologist ensures timely interventions and better long-term outcomes.
Surgical Procedures for Heart Failure
- Coronary Artery Bypass Surgery: Reroutes blood flow around blocked arteries to improve oxygen supply and alleviate symptoms, a critical component of heart failure treatments.
- Implantable Cardioverter-Defibrillator (ICD): Prevents sudden cardiac arrest by monitoring and correcting irregular heart rhythms.
- Heart Valve Repair or Replacement: Improves blood flow and reduces the heart’s workload.
- Heart Transplant: In severe cases, provides a new, healthy heart for patients unresponsive to other treatments.
Devices for Heart Failure
For advanced cases, medical devices are often essential to support the heart’s function. These devices include:
- Pacemakers: Regulate slow heart rhythms, improving blood flow and reducing symptoms of heart failure.
- Implantable Cardioverter Defibrillators (ICDs): Monitor and correct dangerous heart rhythms.
- Left Ventricular Assist Devices (LVADs): Help the heart pump blood effectively in severe cases.
- Cardiac Resynchronization Therapy (CRT): Improves coordination between the heart’s chambers for better pumping efficiency.
These devices, combined with lifestyle changes and medication, form a comprehensive approach to heart failure treatments, especially for patients requiring advanced intervention.
Prevention of Heart Failure
Preventive measures play a vital role in reducing the risk of developing heart failure. Key strategies include:
- Healthy Lifestyle: A balanced diet rich in fruits, vegetables, and whole grains supports heart health.
- Regular Exercise: Activities like walking, swimming, or yoga improve cardiovascular efficiency.
- Managing Chronic Conditions: Controlling high blood pressure, diabetes, and cholesterol prevents strain on the heart.
- Avoiding Harmful Habits: Quit smoking and limit alcohol consumption.
By integrating these preventive actions, individuals can lower the chances of developing chronic heart failure symptoms.
Conclusion
Heart failure is a complex condition that can disrupt daily life, but with the right heart failure treatments, individuals can manage symptoms and enhance well-being. At Dr. Kathiresan’s clinic, we take a personalized approach to heart failure treatments, including the treatment of anemic heart failure, helping patients strengthen their heart, alleviate symptoms, and support long-term health. By understanding the underlying causes, recognizing symptoms, and exploring various treatment options, patients can actively manage chronic heart failure symptoms for a better quality of life.

