When it comes to diagnosing and treating cardiovascular conditions, medical advancements have provided interventional cardiologists with an array of tools and techniques. Among these, two prominent methods stand out: Fractional Flow Reserve FFR vs angiography. While both play crucial roles in assessing coronary artery health, they serve distinct purposes.
In this blog, we’ll delve into the differences between FFR and angiography, exploring their benefits and helping you understand how they work together to guide effective treatment decisions.
What is FFR?
Fractional Flow Reserve (FFR) is a crucial diagnostic tool used to evaluate blood flow in coronary arteries. It helps determine the significance of narrowed arteries, guiding treatment decisions in patients with coronary artery disease. Here are some key points about FFR:
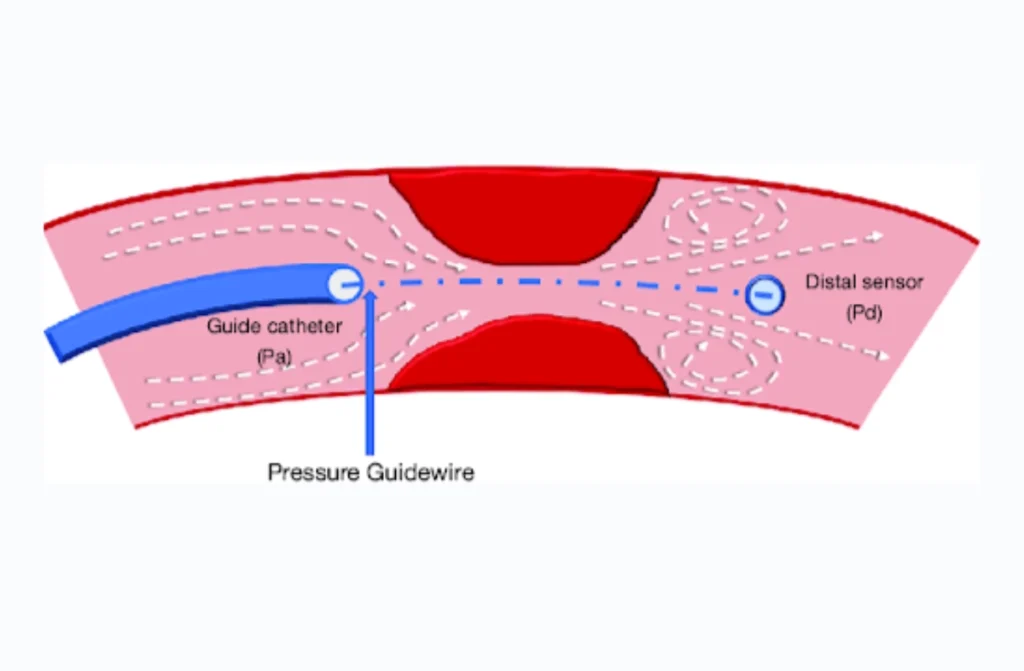
- Pressure Measurement: FFR measures the pressure differences across a coronary artery lesion during maximum blood flow, typically induced by a medication.
- Calculation: The FFR ratio is calculated by dividing the pressure downstream of the blockage by the pressure upstream, providing insights into blood flow efficiency.
- Clinical Significance: An FFR value of 0.80 or lower indicates significant blockage, which may require interventions like stenting, while values above 0.80 suggest the lesion is less critical.
- Comparison: When discussing FFR vs angiography, it’s essential to note that angiography provides visual imaging, whereas FFR quantifies the functional impact of a blockage, offering a more detailed assessment.
- Impact on Treatment: Utilizing FFR in conjunction with interventional angiography can enhance decision-making in cardiac care, improving patient outcomes.
What is Angiography?
Interventional Angiography, also known as coronary angiography, is a critical imaging technique that allows healthcare professionals to visualize the inside of blood vessels, particularly the coronary arteries, which deliver blood to the heart. The procedure involves the insertion of a catheter, usually in the groin or wrist, through which a contrast dye is injected directly into the coronary arteries. This dye highlights the arteries on X-ray images, enabling doctors to identify blockages, stenosis (narrowing), and other vascular issues that may be affecting the heart’s blood supply.
Angiography is an essential tool for diagnosing coronary artery disease (CAD), as it provides clear, real-time images that show the exact location, size, and severity of blockages. This anatomical visualization helps doctors understand the extent of the damage, and in many cases, it guides the decision-making process for further interventions such as stenting or bypass surgery.
Key Features of Angiography
- Visualization: Delivers detailed images of the coronary arteries to assess their condition.
- Diagnostic Tool: Helps locate and measure the severity of blockages, which is crucial for determining treatment options.
- Guides Treatment: Assists in deciding whether surgical procedures, such as stenting or bypass surgery, are required.
While angiography offers valuable structural information about the coronary arteries, it falls short in assessing the functional impact of arterial blockages on blood flow. This is where Fractional Flow Reserve (FFR) comes into play, offering a more comprehensive view of how these blockages affect heart function.
Understanding Interventional Angiography: Visualizing Blood Vessels
Angiography is a widely used diagnostic procedure that involves injecting a contrast dye into the arteries and capturing X-ray images (angiograms) to visualize blood vessel structures. In the context of cardiovascular health, coronary angiography is used to examine the coronary arteries that supply blood to the heart muscle. By identifying blockages, narrowing, or abnormalities in these arteries, cardiologists can diagnose conditions like coronary artery disease (CAD).
The key difference between FFR vs angiography is that while angiography provides valuable anatomical information, it doesn’t provide insights into the functional significance of any detected blockages. This is where Fractional Flow Reserve (FFR) comes into play.
Exploring Fractional Flow Reserve (FFR): Measuring Blood Flow
FFR is a functional measurement that assesses the blood flow within a coronary artery. It’s calculated by measuring the pressure before and after a narrowing or blockage in the artery while a vasodilator is administered. This measurement helps determine if a detected blockage is actually causing a reduction in blood flow to the heart muscle. An FFR cardiac value of 1 indicates normal blood flow, while values less than 1 suggest a significant reduction in blood flow due to the blockage.
The major advantage of FFR Vs angiography is its ability to guide treatment decisions by pinpointing lesions that are truly causing reduced blood flow and those that can be managed conservatively. This helps cardiologists determine whether a stent or other intervention is necessary or if medical therapy and lifestyle changes are sufficient.
FFR vs Angiography: A Collaborative Approach
When it comes to diagnosing and treating coronary artery disease, FFR Vs angiography complement each other. Interventional angiography provides the visual roadmap of the coronary arteries, identifying potential trouble spots. It’s the initial step in evaluating the overall condition of the arteries. However, angiography alone cannot reliably determine the functional significance of a blockage.
On the other hand, in FFR Vs angiography, FFR adds the functional dimension to the diagnosis. By measuring blood flow, it helps cardiologists differentiate between lesions that are causing significant blood flow reduction and those that are not. This prevents unnecessary interventions, reducing the risk of complications and ensuring that patients receive appropriate treatment based on their individual needs.
FFR vs Angiography: A Comparison
| Feature | Interventional Angiography | Fractional Flow Reserve (FFR) |
|---|---|---|
| Primary Focus | Visualizing anatomical blockages in arteries | Assessing the functional impact of blockages on blood flow |
| Method | X-ray imaging with contrast dye | Pressure measurement across the blockage during angiography |
| Purpose | Identify location, size, and severity of blockages | Determine whether a blockage affects blood flow enough to require treatment |
| Application | Guides decisions for stenting or bypass surgery | Helps decide if stenting or other interventions are necessary |
| Invasiveness | Invasive, requiring catheter insertion | Minimally invasive, performed alongside angiography |
FFR Cardiac Cath
Fractional Flow Reserve (FFR) cardiac cath is a specialized procedure to assess blood flow in coronary arteries and identify blockages that may cause significant issues. Using FFR cardiac cath alongside angiography enhances diagnosis by measuring pressure differences across narrowed arteries, guiding decisions on interventions.
- Guided Measurements: Determines precise blood flow restriction.
- Targeted Intervention: Helps identify when angioplasty or stenting is necessary.
- Improved Outcomes: Reduces unnecessary procedures by pinpointing severe blockages.
By using FFR, cardiologists ensure that only essential treatments are pursued, improving patient care outcomes.
Interventional Angiography
Interventional angiography is an imaging procedure that uses contrast dye and X-rays to visualize blood vessels and diagnose blockages, aneurysms, or other issues. This minimally invasive technique often leads directly to treatment within the same procedure, such as stent placement or balloon angioplasty, based on findings.
- Real-Time Imaging: Provides immediate feedback for accurate diagnosis.
- Minimally Invasive: Typically involves a small incision, offering faster recovery.
- Dual Purpose: Diagnoses and treats within one session, streamlining care.
Both FFR cardiac cath and interventional angiography offer a comprehensive approach to managing coronary artery disease, helping patients receive personalized, effective treatment.
The Role of the Defer Trial FFR in Cardiac Diagnostics
The Defer Trial FFR has been a pivotal study in the field of interventional cardiology, providing significant insights into the use of Fractional Flow Reserve (FFR) for guiding treatment decisions. Before the Defer trial, doctors often made decisions about stenting or bypass surgery based solely on the appearance of blockages in angiography. However, the Defer Trial FFR showed that not all blockages identified by angiography need to be treated immediately.
The study demonstrated that if the FFR measurement reveals that a blockage does not significantly affect blood flow (FFR greater than 0.80), there is no need for immediate intervention. This finding was groundbreaking, as it led to a more conservative, patient-specific approach to treating coronary artery disease. By using FFR to guide decisions, healthcare providers can avoid unnecessary procedures, reduce patient risk, and lower healthcare costs.
Key Takeaways from the Defer Trial FFR:
- The trial confirmed that FFR measurements provide critical functional information that angiography alone cannot offer.
- It demonstrated that coronary stenosis with an FFR > 0.80 does not always require immediate intervention, emphasizing a more personalized, conservative treatment approach.
- The Defer Trial FFR established that Fractional Flow Reserve should be used as a tool to guide treatment decisions, potentially avoiding unnecessary stenting or bypass surgery.
Benefits of FFR Vs Angiography
The benefits of considering FFR Vs angiography include:
- Accurate Diagnosis: Angiography offers a clear view of the anatomy, while FFR provides functional data, leading to a more accurate diagnosis.
- Informed Treatment Decisions: FFR cardiac guides cardiologists in deciding whether a stent is required, optimizing treatment strategies.
- Reduced Interventions: FFR prevents unnecessary stent placement, reducing the risk of complications and healthcare costs.
- Personalized Care: The combined use of FFR cardiac and angiography allows for personalized treatment plans tailored to each patient’s unique condition.
When Would Fractional Flow Reserve Be Needed?
Fractional Flow Reserve (FFR) is a diagnostic technique employed during coronary angiography to assess the physiological significance of coronary artery stenoses. FFR is particularly valuable when angiographic findings are inconclusive or when the severity of a lesion is borderline.
Indications for FFR Measurement:
- Intermediate Lesions: For coronary lesions with 50-70% diameter stenosis, FFR helps determine if the lesion is functionally significant.
- Assessment of Ischemia: In patients with symptoms of myocardial ischemia but non-diagnostic non-invasive tests, FFR provides objective data to guide treatment decisions.
- Multivessel Disease: In cases of multivessel coronary artery disease, FFR aids in identifying the most critical lesions that require revascularization.
- Post-Intervention Assessment: After procedures like rotational atherectomy, FFR can evaluate the success of the intervention and the need for further treatment.
FFR measurement involves the use of a pressure wire to compare the pressure distal to the stenosis with the pressure in the aorta, providing a ratio that quantifies the impact of the lesion on coronary blood flow.
When Should I Call My Doctor?
After undergoing rotational atherectomy or any coronary intervention, it’s crucial to monitor for potential complications. Contact your healthcare provider promptly if you experience:
- Chest Pain: Persistent or worsening chest discomfort may indicate complications.
- Shortness of Breath: Difficulty breathing could signal cardiac issues.
- Dizziness or Lightheadedness: These symptoms may suggest hypotension or arrhythmias.
- Fever: An elevated temperature could indicate infection.
- Pain at Access Site: Severe or increasing pain at the catheter insertion site warrants evaluation.
- Palpitations: Irregular heartbeats should be assessed by a healthcare professional.
- Timely communication with your doctor can help address any concerns and ensure optimal recovery.
Conclusion
In the realm of interventional cardiology, FFR Vs angiography are not competitors but allies. They work hand in hand to provide a comprehensive understanding of a patient’s coronary health. While interventional angiography gives us the “where,” FFR answers the “why” by evaluating blood flow dynamics. This collaborative approach ensures that patients receive the most appropriate and effective treatment, minimizing unnecessary interventions and maximizing positive outcomes.
Also Read Intracoronary Physiology – FFR, IFR, RFR.

